Long known as the "king of cancers" due to its abysmal early detection rate, pancreatic cancer is now facing a breakthrough from Chinese AI screening technology. Developed by Alibaba DAMO Academy, the PANDA model can detect cancerous signs in non-contrast CT scans, helping doctors identify multiple cases of early-stage pancreatic cancer.
However, AI early screening is not equivalent to diagnosis, as it still grapples with false positives, communication challenges, and heavy reliance on professional physicians. Future efforts will focus on multi-modal data fusion.
"You Have the Same Disease as Steve Jobs, But You're Much Luckier"
Qiu, a 57-year-old retired bricklayer from Ningbo, Zhejiang Province, recalled to a reporter from the National Business Daily (NBD): In August 2025, he underwent a routine abdominal non-contrast CT scan at the Affiliated People's Hospital of Ningbo University due to diabetes.
During lunch, he received a call from the hospital: "There might be an issue with your pancreas; further examination is needed."
On the other end of the line was Zhu Kelei, vice president of the hospital and chief physician of hepatobiliary and pancreatic surgery. Though the doctor didn’t specify the problem, Qiu knew "it couldn’t be good news."

Zhu Kelei Photo/provided to NBD
He promptly underwent an enhanced MRI and minimally invasive surgery the next day.
Dr. Zhu told Qiu: "You have the same disease as Steve Jobs, but you’re much luckier than him."
Qiu was discharged on the ninth day after surgery. After medical insurance reimbursement, he paid only 12,000 to 14,000 yuan (about $1,680 to $1,960) out of pocket.
Qiu emphasized that he had no symptoms at the time and never imagined he would be diagnosed with pancreatic cancer.
The lifesaver was the PANDA AI early screening model for pancreatic cancer, developed by Alibaba DAMO Academy. This AI system detected cancerous signs in his seemingly normal non-contrast CT images.
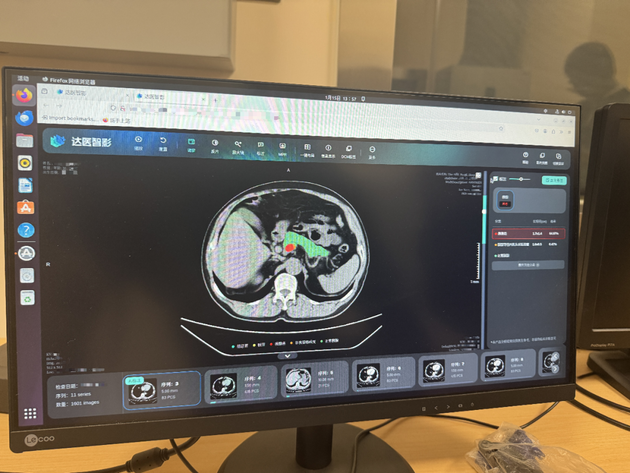

Interface of the PANDA model Photo/Zheng Yuhang (NBD)
Since the PANDA model was deployed at the Affiliated People's Hospital of Ningbo University in November 2024, it has analyzed over 180,000 CT images and helped doctors identify 24 pancreatic cancer cases, 14 of which were in the early stages. Among these 14 early-stage patients, 11 had no abnormal prompts in their initial non-contrast CT reports—diagnosis was only possible after AI alerts led to further examinations.
"AI saved their lives," Dr. Zhu stated. "They all came to the hospital for other illnesses, not pancreatic specialists. Most of their CT scans showed no abnormalities, and it was AI that ‘sounded the alarm.’"
How Can AI Detect What Doctors Miss?
When Alibaba DAMO Academy’s medical AI team decided to pursue "non-contrast CT + AI" for pancreatic cancer screening in 2021, they faced skepticism: "If doctors can’t detect it, how can AI label and train the model?"
Dr. Zhu explained that clinically, abdominal CT scans are divided into non-contrast and enhanced CT. Enhanced CT requires patients to receive contrast agents, providing clearer images of organs and lesions, but it is more costly, complex to perform, and carries a risk of allergic reactions—typically reserved for patients with specific diagnostic needs.
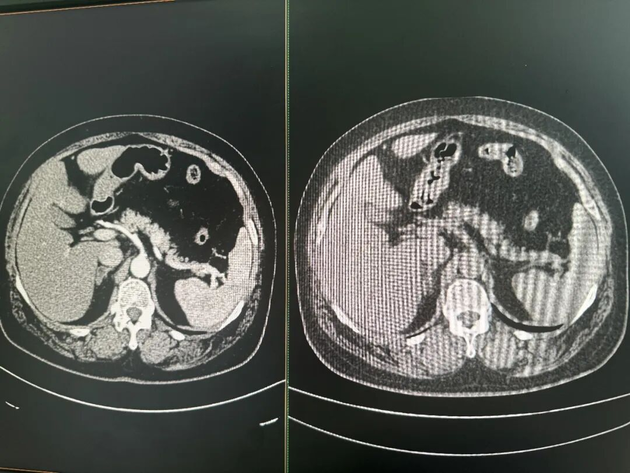
Comparison of contrast-enhanced CT (left) and non-contrast CT (right) images Photo/Zheng Yuhang (NBD)
In contrast, non-contrast CT is affordable and widely used, serving as one of the most common imaging tools in routine physical exams and outpatient visits.
However, due to the low contrast between the pancreas and surrounding tissues, it is difficult to visualize on non-contrast CT scans. Tiny early-stage tumors are practically "invisible" and extremely hard to detect with the naked eye. Thus, "non-contrast CT cannot be used for early pancreatic cancer screening" was once a universal consensus among radiologists.
Zhang Ling, algorithm director of medical AI tumor early screening and imaging intelligence at DAMO Academy, clarified: CT images are essentially a sequence of continuous values ranging from -1024 to 1024, with different values corresponding to tissues of varying densities. Many details exceed the limits of human vision but can theoretically be distinguished through data and algorithms.
To address this, the team adopted a "roundabout strategy":
They collected data from thousands of pancreatic cancer patients. Experienced doctors first accurately labeled lesion locations on clear enhanced CT images, then used image registration technology to precisely "map" these labels back to the same patients’ non-contrast CT images.
After nearly two years of training, the PANDA model learned to identify subtle density changes, textural abnormalities, and structural distortions in non-contrast CT scans—features imperceptible to the human eye but telltale signs of early pancreatic cancer.
Data from a paper published in the international top journal Nature Medicine in November 2023 showed that the PANDA model achieved a sensitivity (ability to detect lesions) of 92.9% and a specificity (ability to exclude non-lesion cases) of 99.9% for pancreatic cancer screening. This means AI can not only identify most patients but also avoid large-scale "false alarms."
In April 2025, the U.S. Food and Drug Administration (FDA) granted the PANDA model the "Breakthrough Device Designation."
AI Early Screening ≠ AI Diagnosis: Heavy Reliance on Professional Doctors
Despite its 99.9% specificity in laboratory settings, the journey from AI alert to final patient diagnosis faces numerous hurdles in complex real-world clinical applications.
Reporters discovered that technical limitations, unavoidable false positives, and resulting doctor-patient communication barriers pose significant challenges to the implementation of AI early screening.
Shen Yiyu Photo/Zheng Yuhang (NBD)
Shen Yiyu, director of general surgery at Jiaxing No.2 Hospital, emphasized: "AI early screening is not diagnosis."
Approximately 600 to 700 CT scans are analyzed by the AI model at his hospital daily, with around 20 images flagged for potential pancreatic issues. Radiologists and hepatobiliary-pancreatic surgeons conduct two rounds of manual review to determine which patients need follow-up examinations.
"I now spend a lot of time figuring out how to recall patients," Dr. Shen admitted. Initially, he and his team tried calling patients directly on their personal phones, but "more than half hung up immediately," mistaking the calls for spam or fraud.
When doctors straightforwardly told patients, "There’s a problem with your pancreas; you need to come back for a follow-up," reactions were often intense: "Are you crazy? Are you cursing me? My stomach doesn’t hurt, and your hospital’s report said everything was normal—why are you calling me back?" Some even accused the hospital of "seeking profits" or "scamming money."
To build trust, the team systematically improved communication processes. The hospital established a dedicated consultation hotline and assigned specialists to address patient inquiries.
Even so, the follow-up recall rate improved slowly. Dr. Shen’s data showed that initially, only about 10% of patients requiring follow-up returned. After over a year of process optimization, this rate rose to 25% by the end of 2025. "We identified more than 1,300 patients needing follow-up, but only over 300 came back."
When asked about false positives in practical applications, doctors remained cautious. Industry insiders acknowledged that given the low incidence of pancreatic cancer, the PANDA model theoretically carries a small risk of false positives. "False positives not only cause unnecessary patient panic but also waste medical resources. The positive predictive value of the PANDA model in real-world scenarios requires long-term data accumulation."
Beyond false positives and communication issues, the technology itself has room for improvement. Currently, the PANDA model’s core technical path focuses on computer vision (CV) and has not yet achieved deep multi-modal data fusion.
"The entire AI industry is moving toward multi-modality, which is our core direction for the future," an insider noted. "Integrating CT imaging data with patient medical records, biochemical indicators, and other multi-dimensional information will further enhance the system’s accuracy."
Additionally, the model’s performance heavily depends on the doctors using it. In the hands of experienced physicians, PANDA becomes a powerful auxiliary tool, but its effectiveness may diminish when deployed to less experienced doctors in primary hospitals.
Model development also relies on continuous feedback from doctors. From the initial 1.0 version, which only provided red-yellow-green risk alerts and simple lesion outlining, to the 2.0 version that better distinguishes pancreatitis from other lesions, clinical feedback has been crucial for algorithm optimization. Even today, it remains a system that continuously learns and evolves through real-world application.
The Economic Case for AI Early Screening
Beyond saving lives, AI early screening for pancreatic cancer also generates substantial cost savings for patients. Dr. Shen broke down the numbers:
Early-stage patients: Total costs from surgery to recovery are approximately several tens of thousands of yuan before insurance. (In Qiu’s case, out-of-pocket expenses were less than 15,000 yuan after reimbursement.)
Late-stage patients: Most miss the window for surgery upon diagnosis. Treatment costs range from hundreds of thousands to over a million yuan, with limited efficacy—median survival is less than a year.
This imposes a heavy burden on families, medical insurance funds, and society as a whole.
"If I told you there’s an injection that could extend your loved one’s life by three to four months, but costs 1 million yuan per shot—would you sell your house to afford it?" Dr. Shen posed a rhetorical question. Pancreatic cancer can push an average family into poverty, with no guarantee of a cure.
Dr. Zhu emphasized that AI early screening can significantly increase early detection rates and reduce overall treatment costs: "The economic benefits are clear." However, current AI screening remains "opportunistic"—it only works when patients undergo CT scans for other illnesses. "If patients don’t visit the hospital, AI has no way to detect risks."
Dr. Zhu proposed deploying the AI alert model directly on regional health big data platforms. Yinzhou District, where he practices, is one of the first regions in China to establish a resident health database, aggregating data for over 1.4 million permanent residents.
"I envision integrating imaging, blood, and tumor marker data to build a more accurate model," Dr. Zhu explained. In this model, AI would transform from a "passive catcher" to an "active sentinel."
For example, if a resident’s blood sugar spikes during a checkup at any hospital in Zhejiang Province, AI could access their health records, discover a tiny pancreatic lesion, and integrate these seemingly unrelated pieces of information to generate an alert: "Your health risk is increasing—please undergo specialized examination at a hospital promptly."
"This is equivalent to installing an alarm for every resident in our jurisdiction," Dr. Zhu stressed. This proactive alert system would no longer be limited to single CT scans but would continuously monitor and analyze multi-dimensional, cross-temporal, and cross-regional health data, enabling early warnings before illness onset or at the earliest stages.


 川公网安备 51019002001991号
川公网安备 51019002001991号